Kitsap County COVID-19 Guidance for Homeless SERVICE Providers
First, we want to thank you so much for all your work to keep the homeless shelters and day rooms open during this incredibly challenging time. We know this is never easy, and that the heightened uncertainty and new realities of day to day life are making it even more difficult.
Last updated 8/5/2020 9am
Recent Updates
We will post recent news, changes, or updates as they become available here.
Quarantine and Isolation for Community Based Organizations
Guidance for Community Based Organizations has been released to provide information about the referral process when guests or clients living in congregate or communal living situations and have symptoms of COVID-19.
See the flowchart and guidance here.
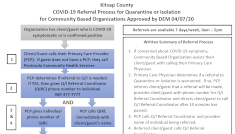
Quarantine and Isolation Flowchart for Community Based Organizations(updated 8/52020)
Kitsap Public Health District Shelter Recommendations and Contact Tracing
Kitsap Public Health District has developed the COVID-19 prevention recommendations for Kitsap homeless shelter providers. These recommendations incorporate the latest guidance from the Center for Disease Control and should replace any prior guidance or recommendations that are less stringent. They are focused on preventing the spread of COVID-19 and assisting KPHD to do contact tracing in the event of a possible COVID-19 case in a shelter facility. These recommendations have been merged into the guidance provided below on this page.
 KPHD Shelter Recommendations (5/8/2020)
KPHD Shelter Recommendations (5/8/2020)
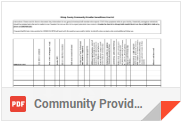 Kitsap County Community Provider Surveillance Line List (5/11/2020)
Kitsap County Community Provider Surveillance Line List (5/11/2020)
Shelter/Day Room Guidance: COVID-19 Precautions
At this point, our best tools in preventing the spread of COVID-19 are simple ones:
Stay calm.
Wash hands often for 20 seconds using soap/water or use alcohol-based sanitizer. Everyone should wash upon entering a facility and before and after using the restroom or eating.
All guests/visitors should wear face coverings or masks when not in their rooms or at their bed cot/mat. Staff and volunteers should wear masks at all times.
Cover coughs and sneezes with an elbow or tissue. Throw tissues away immediately.
Avoid close contact with people who are sick, avoid hugs, touching, keep a distance of 6 feet.
Clean and disinfect frequently-used objects and surfaces.
Stay home when sick and avoid close contact with others.
How these precautions apply to Shelters and Day Rooms
Below are some recommendations for modifications to check-in procedure, based on the best-known information at this time from local and state health departments. These steps and changes will vary site to site depending on the layout of the facility and the availability of supplies. To the extent possible:
Modifications to Check-in/Entry/Visitation Procedures
Collect contact information for all shelter guests and visitors. Use a sign-in sheet that includes date, time, and best way to contact (cell phone, email, message phone, Facebook Messenger, etc.) prior or upon entry to the facility.
Ask screening questions (see next section), check temperature, and encourage guests to report illnesses and exposure to COVID-19 to staff
prior or upon entry to the facility. If guests have symptoms or a temperature above 100.0°F, initiate the
COVID-19 Referral Process for Quarantine or Isolation for Community Based Facilities. If visitors have symptoms or a temperature they should be turned away.
Staff, volunteers, guests, and visitors should
wash their hands
or use hand sanitizer for 20 seconds before signing-in, entering the common areas, and before and after using the restroom or eating. (How long is 20 seconds?" The time it takes to hum or sing the
ABC's or
Twinkle Twinkle Little Star.)
Provide options to increase social distancing at the check-in area and throughout common areas. Have staff, volunteers, and guests keep extra space, at least 6 feet apart, between people wherever possible.
Provide tissues, trash receptacles, and washing stations or hand sanitizer in waiting areas. Encourage everyone in the facility to cover their cough or sneeze with a tissue and have trash cans available to dispose of tissues immediately.
All guests and visitors should wear cloth face coverings any time they are not in their room or on their bed/mat (in shared sleeping areas). Cloth face coverings should not be placed on young children under age 2, anyone who has trouble breathing, or is unconscious, incapacitated or otherwise unable to remove the mask without assistance. Staff and volunteers should always wear cloth face coverings or masks.
Clean and disinfect frequently touched surfaces - see guidance under the topic "Cleaning, Disinfecting, and Sanitizing"
Screening Questions and Responses:
To minimize the length of time a contagious person may be within a facility, screen guests and visitors upon entry and at elast once per day:
-
1.Determine if the guest has a fever by:
- Taking their temperature using an infrared or temporal thermometer, or
- Asking the question "Have you felt like you had a fever in the past day?"
-
2.Ask the guest "Do you have a new or worsening cough today?"
-
3.Ask the guest "Are you experiencing any other symptoms of illness?"
- Less common symptoms of COVID-19 or other symptoms include chills, muscle pain, sore throat, headache, and new loss of taste or smell. Seek medical attention is the guest reports trouble breathing, pain or pressure in the chest, confusion or inability to arouse, or bluish lips or face.
*This is not a comprehensive list of symptoms of acute/severe symptoms requiring medical attention.
If a guest has a temperature above 100.0°F OR a new/worsening cough OR 2 or more of the less common COVID-19 symptoms:
- i.
Provide a face covering or mask for the client to wear over the nose and mouth, if masks are available and if the client can tolerate wearing the covering.
- ii. If masks are not available or the guest cannot wear a mask,
advise the guest to cover coughs and sneezes with a tissue or elbow.
- iii. Separate the guest from the shelter common areas and away from others or to an area designated for symptomatic guests.
- iv.
Notify a manager and initiate the
COVID-19 Referral Process for Quarantine or Isolation for Community Based Facilities.
Quarantine and Isolation Flowchart for Community Based Organizations(updated 8/5/20)
- a.
Assist guest in contacting their Primary Care Provider (PCP). If the guest does not have a PCP contact Peninsula Community Health Services at (360) 377-3776.
- b. The PCP determines if a referral to Quarantine or Isolation is warranted. If so, PCP informs client/guest that a referral will be made, provides client/guest with phone number for Q/I Referral Coordinator and directs client/guest to call Q/I Referral Coordinator after 10 minutes has passed.
-
v.
Notify KPHD using the "Surveillance Line List."
Cleaning, Disinfecting, and Sanitizing
Additional Cleaning: Do additional cleaning of frequently touched surfaces, such as tables, chairs, doorknobs, furniture, bathrooms, light switches, and countertops. Each location may have different cleaning solutions or disinfectants; Program Managers should provide instruction as to the available cleaners at your site and their proper use.
Detailed Guides
Public Education and Information
Information Posters: Posters from the CDC and Health Department regarding COVID-19 should be displayed at check-in areas and other locations around the site. You can download these posters at
https://kitsappublichealth.org/CommunityHealth/CoronaVirus.php
Separation and Isolation
Separation or Isolation: Depending on the physical site, there may be opportunities to provide additional spacing between beds. In general sleeping areas (for guests not experiencing respiratory symptoms), try to make sure clients faces are at least 6 feet apart. Align mats/beds so that clients sleep head to toe. Set up dining chairs at least 6 feet apart. If possible, for symptomatic guests, use separate rooms, spaces, or opposite ends of a room to separate sick guests from other guests without symptoms. Refer to
https://deptofcommerce.app.box.com/v/Covid-19-Shelter-Guidelines/file/635030853862 pages 3-4 for more detailed steps for Isolation Considerations.
If possible, sick clients should be confined to individual rooms with separate bathroom and eating facilities and should avoid common areas. In the bedroom/bathroom dedicated for an ill person consider reducing cleaning frequency to as-needed (e.g., soiled items and surfaces) to avoid unnecessary contact with the ill person.
As much as possible, an ill person should stay in a specific room and away from other people, following
home care guidance.
If individual rooms for sick clients are not available, consider using a large, well-ventilated room specifically for sick persons, especially for people with respiratory disease symptoms.
In isolation areas, help reduce spread by:
Arranging beds at least 6 feet apart
Creating temporary physical barriers between beds using sheets or curtains.
Arranging beds so that individuals lie head to toe relative to each other.
If a separate bathroom is not available, the bathroom should be cleaned and disinfected after each use by an ill person. If this is not possible staff should wait as long as practical after use by an ill person to clean and disinfect the high-touch surfaces.
Personal Protective Equipment (PPE)
FEMA Fact Sheet on PPE Guidance for Non-Medical Sectors
This guidance summarizes how organizations should consider and manage their personal protective equipment (PPE) needs while ensuring the protection of workers during the coronavirus (COVID-19) pandemic response.
 Addressing PPE Needs in Non-Healthcare Setting
Addressing PPE Needs in Non-Healthcare Setting
Staff who do not interact closely (e.g., within 6 feet) with sick clients and do not clean client environments do not need to wear personal protective equipment (PPE).
Staff who are checking client temperatures should use a system that creates a physical barrier between the client and the screener as described
here.
Mask Use for Shelter Guests and Staff
All shelter guests should wear cloth face coverings or masks when not in their rooms or at their bed cot/mat. Staff/volunteers should wear masks at all times.
Cloth face coverings should not be placed on young children under age 2, anyone who has trouble breathing, or is unconscious, incapacitated or otherwise unable to remove the mask without assistance. Cloth face coverings should be treated as hazardous if dirty and should be laundered at least daily. It is okay to launder masks with other clothing/bedding.
See
CDC Guidance regarding Cloth Face Coverings
Shelter staff can demonstrate correct mask use in order to assist guests.
Fit is important
Masks are only effective in their intended use if they are used properly. The following rules must be followed for correct mask use:
The mask should fit snugly over the face.
The colored side of the mask faces outwards.
The strings or elastic bands are positioned properly to keep the mask firmly in place.
The mask covers both your nose and mouth.
The metallic strip is molded to the bridge of your nose.
Putting on and removing masks
Putting on the mask or “donning” - Wash hand before putting on mask. Place the mask over the face, covering the nose and mouth, and secure the ties or ear loops. Adjust the nose piece if the mask has one. Wash hands.
Do not touch or readjust the mask if possible, if readjustment is necessary wash before hands before and after adjusting the mask.
Removing the mask or “doffing” – Wash hands before touching the mask. Consider the mask contaminated, remove the mask by the ear loops or ties, touching the mask as minimally as possible. Do not touch eyes, nose, or face. Discard disposable masks into garbage, or cloth masks into receptacle. Wash hands.
Staff Considerations
Screen staff and volunteers for symptoms and check temperature at the start of each shift. If staff have symptoms or a temperature above 100.0°F, they should be sent home immediately. If symptoms develop while at work, the individual should isolate immediately and return home as soon as possible. If this occurs notify KPHD using the Kitsap Shelter Surveillance Line List.
Plan for staff and volunteer absences. Staff (and volunteers) may need to stay home when they are sick, caring for a sick household member, or caring for their children in the event of school dismissals.
Encourage ill staff and volunteers to stay home (or be sent home if they develop symptoms while at the facility), to prevent transmitting the infection to others.
Staff and volunteers who are at
higher risk for severe illness from COVID-19 should not be designated as caregivers for sick clients who are staying in the shelter. Identify flexible job duties for these higher risk staff and volunteers so they can continue working while minimizing direct contact with clients.
Plan your staffing to minimize the number of staff members who have face-to-face interactions with clients with respiratory symptoms.
Maintain an on-site list for staff and volunteer with their "best way to contact" info.
Staff and volunteers should report if they are working any other jobs in addition to the shelter. Keep a list of these other employers and contact information on-site.
Working with People Experiencing Unsheltered Homelessness
The
Centers for Disease Control and Prevention (CDC) has issues interim guidance is based on what is currently known
about coronavirus disease 2019 (COVID-19). The Centers for Disease Control and Prevention (CDC) will update this interim guidance as needed and as additional information becomes available.
Volunteers Needed
Volunteer Requests
Kitsap County Department of Emergency Management has sent a formal request to recruit volunteer to help staff quarantine/isolation shelter sites for COVID-19 patients in Kitsap County.
Read the formal request here. To apply
complete an application and submit to
volunteer@kitsapem.org. Severe Weather Shelter volunteers do not need to complete the application and may simply email to participate.
There are several shelters looking for volunteers, the Salvation Army, Kitsap Rescue Mission, and City of Poulsbo/Gateway Fellowship day shelter. In additional to these shelters there are quarantine/isolation sites if that is of interest. During the COVID-19 response our Kitsap County Department of Emergency Management is screening volunteers and providing liability coverage through the Emergency Worker program.
Contact information for interested volunteers:
Salvation Army - contact office at (360) 373-5550 or
lance.walters@usw.salvationarmy.org
Kitsap Rescue Mission - contact office at (360) 373-3428 or
aleach@kitsaprescue.org
Gateway Day Shelter - contact the City of Poulsbo volunteer helpline at 360-517-5037
Quarantine and Isolation Sites - volunteer@kitsapem.org
These programs may require you to be screened for the Emergency Worker Program. Complete
an application and email to
volunteer@kitsapem.org

